Howdy Everyone! As we begin opening up various areas with different precautions I wanted to bring attention to a critical piece of the COVID-19 puzzle. So let’s dive into how SARS-CoV-2 spreads in different settings and just how much damage one “Super Spreader” can cause. This is no sexual innuendo but a description of a person who can spread a disease to an unusually large amount of people.
For this post I’ll be pulling some examples from Erin Bromage’s post about The Risks – Know Them – Avoid them as they do a great job reviewing several different super spreading events.
It has been established that someone who has been infected with SARS-CoV-2 is capable of spreading the virus even when they do no feel sick themselves. The current measurements of this disease’s R0, a measurement for the capacity of a disease to spread, range 2 to 6.6 depending on sampling. Precautions such as social distancing and masks can drop the R0 to below 1. This means that without precautions (original R0) one infected person can go on to spread the disease to between 2 and 6 people while with precautions (decreased R0) an infected person may not go on to infect anyone at all.
A super spreader is someone who is able to infect more people than the average carrier. Think of this as the modern term for a Typhoid Mary. Mary Mallon, the Typhoid Mary, was the first recognized super spreader and was an asymptomatic carrier for Typhoid fever. Because Mary never felt sick she continued her profession as a cook and was able to infect 51 people with the disease before the cases were traced her and she was placed under quarantine. While I can’t find the R0 for typhoid, one person infecting 51 others was unheard of at the time. Another early super spreader of typhoid fever, Mr. N. the Milker from England, was able to infect over 200 people in 14 year span.
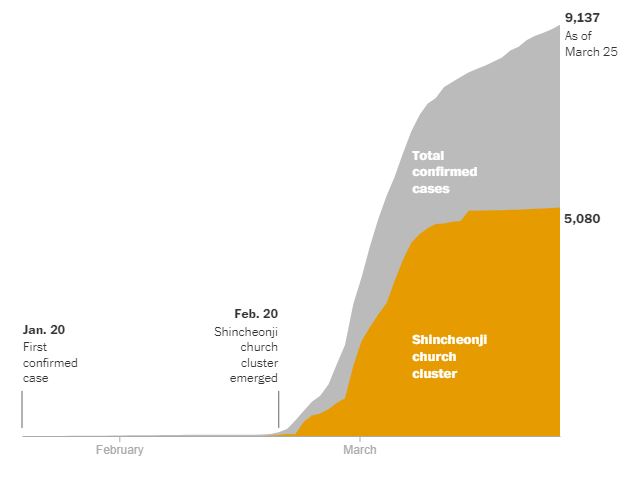
Today we are once again seeing spread from asymptomatic spreaders, carriers of SARS-CoV-2 who don’t feel sick, and these people can have a disproportionate impact within their community. The first known super spreader for COVID-19 was a woman in South Korea who attended church. While it is still unknown how the woman in question contracted the virus, she was able to directly pass the virus to at her church. After attending church just once, the disease spread from the church and made its way into hospitals, elderly care centers, and other churches where people fell sick in droves. Just over one month later, the cluster related to the Shincheonji church accounted for more than half of South Korea’s total 9,137 cases. This one woman managed to make even the famous Typhoid Mary look lazy. [ref]
Closed environments, such as a church, are where we spend a majority of our time outside of the home and one study in Japan found that the disease can spread in a closed environment 18.7 times greater than open-air environments. [ref] A call center in South Korea has become an example of the dangers in a packed workplace environment. One person tested positive for SARS-CoV-2 in an office building. The building was closed immediately and testing was offered to all occupants of the building. Text messages were sent to anyone who spent longer than 5 minutes inside of the building that recommended immediate COVID-19 screening. This resulted in over 1,000 people being tested and identification of 97 people who were positive for the virus. The majority of cases (97%) worked on the same floor. Interestingly the original patient in the building worked on a separate floor and never went to the floor as the majority of people who became sick, it appears that the second person who worked on the floor with high spread caused 93 other people on their floor to become sick. This second person worked in a call center and was able to spread the disease to people all over the floor, shown as the blue desks in the image below. [ref]

The truly sad thing is that super spreaders are an ongoing story all over the world, capable of spreading COVID-19 through churches [ref, ref, ref], hospitals [ref], choir rehearsals [ref], restaurants [ref], and business meetings [ref]. Even family events such as funerals and birthday parties are now opportunities for COVID-19 to spread. [ref] We are beginning to see the virus spread through places where close contact in unavoidable such as meat processing and detention facilities [ref, ref] Without precautions this disease is able to tear through the populations of most of our indoor environments and put everyone young and old, healthy or not at risk of catching the virus.
Because of the risk of asymptomatic carriers and super spreaders, the guidelines for how we deal with this pandemic have changed as we are learning more about this disease. While the recommendations have changed we have continued to narrow down what prevents the spread of COVID-19. A new review out this week shows that consistently wearing masks is the best prevention for slowing the spread of coronaviruses [ref] with gloves, gowns, eye protection, and hand washing also being associated with decreasing the risk for healthcare workers becoming infected. Another study that came out in early April that modeled mask use by the general population and predicts that 80% mask compliance can lower mortality, depending on population density. [ref]
COVID-19 has given us a unique situation where every person is able to contribute to the effort of fighting this disease through small, consistent actions. By washing our hands and wearing our masks when we can, we can all help prevent the spread of this disease and better establish a new normal.
Stay masked and stay safe,
-Your friendly neighborhood scientist