As the spread of COVID-19 increases across the USA we’re seeing a wider variety of patients being admitted into hospitals and ICUs that are younger and healthier than the patients seen in the initial surge across the world. Because these patients have a lower incidence of death we’re starting to see more of the lasting effects that SARS-CoV-2 infection has on the body. While there are no academic papers I can find currently dedicated to the subject, it’s worthwhile to look through various articles to see the outcomes reported in patients who do recover and what their recovery means.
What we know about SARS-CoV-2 Infection
SARS-CoV-2, the virus that causes the disease COVID-19, is spread through respiratory droplets of infected people. Those wearing a mask that properly covers the nose and mouth are much less likely to spread the disease than anyone who is not wearing a mask and anyone properly wearing a mask decreases their likelihood to catch the disease as well. SARS-CoV-2 begins to spread in the upper respiratory system, throat, nose, and pharynx. The virus is does so well in the nasopharynx that it is most sensitive to early detection and why being swabbed for the virus feels like having your brain tickled.
After the virus has colonized the upper respiratory tract it may continue into the lungs and cause a more severe infection. For those that only experience COVID-19 as an upper respiratory infection symptoms may be only as bad as a cold or someone could experience no symptoms at all and be asymptomatic. For those people who have SARS-CoV-2 spread into the lungs they begin to have terrible dry coughs than can progress to pneumonia.
As with all diseases, the initial diagnosis of COVID-19 just means that SARS-CoV-2 has been found in the body. While the disease can be severe for some, in other patients it can be a mild cold; conditions such as asthma, high blood pressure, obesity, among others can increase the likelihood of the disease being more severe but no point of progression is guaranteed for anyone. There’s currently not enough data to allow doctors predict who will become a critical patient and who will be well enough to stay at home to recover. Recent findings that remdesivir and steroids can improve recovery are huge steps forward but they still not enough to decrease the dangers of COVID-19.
SARS-CoV-2 Spike and ACE2
The SARS-CoV-2 virus is able to enter cells by attaching to an angeotensin-converting enzyme 2 or ACE2. ACE2 normally binds to angeotensin II (ANGII) and cuts ANGII thus limiting its affects in the body and can also regulate some traffic passing through the cell membrane. It is the trafficking function that SARS-CoV-2 uses to enter into cells and begin its viral replication process.
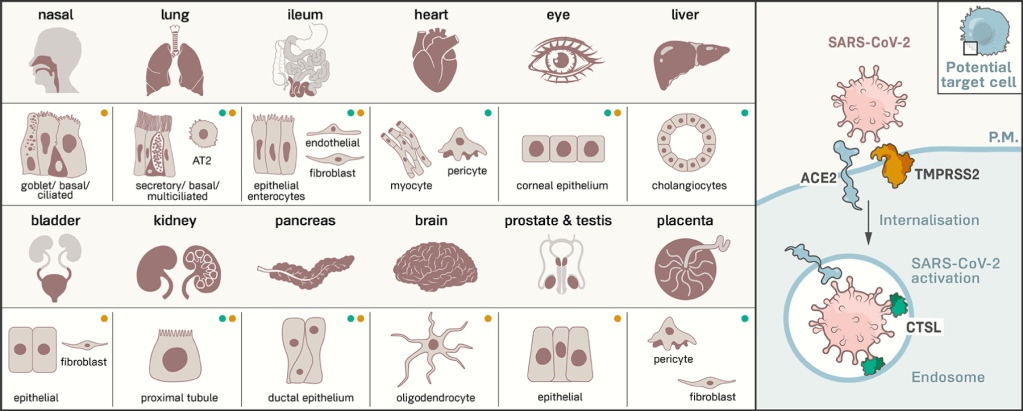
As shown in the grahic, ACE2 is expressed across the body meaning that SARS-CoV-2 could infect much more than respiratory tract tissues. [link] Each of the displayed organs has the potential to be infected with SARS-CoV-2, which is why we are now starting to see more complications with the disease as younger people become infected and survive.
While SARS-CoV-2 infection starts in the lungs it is able to spread to other organ systems from there. Due to the nature of the lung and the means by which we get oxygen into our blood stream there are some thin areas that can become infected and spread the virus into the blood, allowing the virus to spread to every part of the body it can infect.
Lingering Respiratory Problems
Because SARS-CoV-2 starts in the respiratory tract, the lungs can experience extreme trauma from the virus. Damage accumulated from COVID-19 pneumonia could potentially take years to recover from and one patients lungs were so badly damaged she had a double lung replacement [link, content warning for images of the removed lungs]. The patient, in her 20s, had lungs so damaged that the surgery to remove them took longer than expected; images shown of the removed lungs look more like bad hamburger than lungs. Severe damage to the lungs can throw off the body’s normal abilities to regulate itself and can lead to damage to other organs such as the heart and kidneys. Even less severe cases can have damage to the lungs that may take years to recover as there no current way to treat the damage.
Damage to the lungs can lead to acute respiratory distress syndrome (ARDS) which can lead to fluid leaking into the lungs and an overreaction of the immune system called a cytokine storm that can lead to death.
Cardiovascular Problems
From the early days for the COVID-19 outbreak it was known that even after recovering from the virus there was an increased risk from heart attack and stroke. Doctors across the world are commenting that the blood of COVID-19 patients is unusually thick with patterns of vascular damage. This is currently being described as the “second phase” of COVID-19 infection and doctors are currently fighting to figure out how to control the symptoms. [link] These cardiovascular effects are why heart and blood pressure problems were some of the earliest conditions associated with a poor outcome with COVID-19.
With this second phase and thick blood come increased risk of blood clots that can cause heart attacks, strokes, and pulmonary embolisms where blood clots block circulation to the lungs which can cause further damage. All of these experiences can be life threatening for healthy individuals and are very dangerous to those who have already been weakened by COVID-19. There’s little to no data that’s been released on the frequency of occurrences or what about COVID-19 is causing blood clotting, but even if there is no causation the correlation between COVID-19 and blood clots is concerning. [link]
Other COVID-19 Impacts
The nervous system is also a target for COVID-19 and a French study found that a majority of critically ill patients also experienced some form of neurological symptoms during their time at the hospital. [link] Beyond the risk for stroke, it is possible that due to the stress people can develop psychiatric disorders after COVID-19 or see more symptoms from disorders previously diagnosed. [link] Confusion is one theme that is spread across several different reports but it could be due to the drugs necessary to maintain intubation in the most severe COVID-19 cases.
Kawasaki disease attributable to COVID-19 is showing up in children who present with swollen hands and feet, while only some children who present test positive for SARS-CoV-2 the numbers of children with these symptoms outpace normal frequencies and the correlation between COVID-19 and Kawasaki are being looked into. [link] If COVID-19 is related to these new presentations of Kawasaki disease it is likely because of SARS-CoV-2 infecting blood and possibly vessels and allowing fluid to escape from circulation into the body.
The final complication I wish to address is possible damage to kidneys. I’ve seen more posts being shared on social media where adults (20-40 years old) claim to have recovered from COVID-19 are told they need dialysis for at least the short term and possibly the rest of their lives. It’s not currently clear if COVID-19 is directly affecting the kidneys or if the thickened blood, cytokine storm, or oxygen starvation are having an indirect affect. Whether people are able to regain kidney function is currently unknown but presents a risk even to the young, healthy adult that becomes infected.
Staying Safe
COVID-19 has the rare ability to wreak havoc across the entire body from damage to the brain via stroke all the way down to causing swelling in the toes. With so many younger people becoming sick during the current peak in the US we will soon see people released from hospitals who have possible years of recovery in front of them before they are able to function normally. The best thing for everyone to do is to stay home as much as possible and wear masks when you go out.
The more people wear masks, the faster we can get back our outdoor activities. Based on data that suggests massive protests didn’t create COVID-19 spreading hotspots because of mask use, it’s possible that we could resume more of our outdoor activities when mask use becomes the norm. Imagine, we could be back in sports arenas and at festivals and farmers markets again this fall if we all do well now.
Good luck out there,
-Your friendly neighborhood scientist